By Michael Rizk, CPT, ART
Have you ever witnessed a relationship gone sour? The telltale signs are significant, but many
times the root cause stems from poor communication. There is one particular area of the body
that seems to get more press than a short‐lived Hollywood hook‐up. You’ve got it – the lumbar
spine (LS) is likely the most injured, dysfunctional, and (supposedly) weakest link of the body.
In relation to the rest of the body, the LS is active in nearly every functional task performed … it
resides at the crossroads of the body. For that reason, it is important for the rest of the body to
communicate with the low back to let it know how important it is, how much it is needed, and
how much it is appreciated for all it does.
What is meant by communication with the LS? Great question! Communication refers to the
ability of all our joints to feed triplane motion to the LS creating triplane stability. A lack of
triplane mostability (mobility plus stability) can shut down the phone lines feeding
proprioceptively rich information to the LS, thus creating undesirable chain reactions.
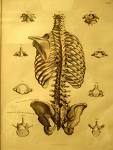
By design, the LS facilitates flexion and extension, allows lateral flexion, and almost inhibits
transverse plane motion. The small amount of transverse plane motion may in fact be the most
important motion allowing the LS to be the transverse plane transmitter of forces between the
upper and lower extremities.
To simplify motion, we consider two phases: loading and unloading. Loading is the preparation
of the task and unloading is the performance of the task. Using the golf swing as an example,
the backswing is the load and the downswing / follow through is the unload. The moment of
time between the load and unload is what we call the transformational zone (TZ). The TZ is
where motion is decelerated and transformed into a concentric production of force.
Understanding what happens just as we enter and exit the TZ will allow us to effectively assess
our patients and clients.
I recently assessed a 57‐year‐young right‐handed golfer with right low back pain, which
occurred during the end range of his back swing just prior to transition. His approach to me was
simple, “So I heard you can fix my back.” With a humble smile, I explained how the body works
relative to the intended task. I shared with him how a lack of three‐dimensional motion
(communication) at any segment will become excessive compensatory motion elsewhere.
While his assessment started with a gait evaluation, I kept in mind that gait and golf create very
different chain reactions in the TZ. During gait, the pelvis and trunk move opposite each other,
and in golf, they move in the same direction. However, I immediately noticed an inability to
load the left side of his body during gait, which was evident by a rough transition from his right
to left foot, as well as an early heel rise on the left foot. After viewing this global glitch, I had to
become a biomechanical detective and get more specific.
To further assess his left ankle and left hip, I had him perform a three‐dimensional balance
reach matrix. He lacked balance when I asked him to reach in the frontal and transverse planes
from his left foot. To create stability, I placed him in the TRUEStretch™ in a backswing posture
and had him perform his balance reaches from this golf‐specific position. Lo and behold, he said
“Wow, it feels like my ankle doesn’t want to turn that way!” He continued to say, “I wonder if
the left ankle sprain I had playing college basketball has anything to do with this?”
Next, I positioned him in his backswing posture to his threshold of success (meaning prior to
experiencing any pain or compensation) and used my hands as a driver to facilitate frontal and
transverse plane subtalar joint (STJ) motions. To balance his new mobility with stability, we
performed lateral and rotational lunges with three‐dimensional arm drivers specific to the golf
TZ. This strategy facilitates proprioceptive communication between his left STJ and right LS.
Within one week, my client was enjoying a pain free backswing with added yardage and accuracy. Needless‐to
say, we were both happy. Even though my client came to me with low back pain, I am led to believe his lack of frontal and
transverse plane motions at his left STJ was, at least, in part the CAUSE of his LS dysfunction. If
we take a snapshot of the backswing, we can see the following: right trunk rotation, right hip
internal rotation, left hip external rotation, right ankle inversion, and left ankle eversion. Frontal
plane eversion of the left STJ transforms into rotation of the left limb; therefore, a lack of that
motion must be made up somewhere else in the kinetic chain. With the nominal amount of LS
rotation available there, is not much room to compensate at the LS before dysfunction and pain are experienced.
With an understanding of Applied Functional Science (AFS) and chain reaction biomechanics we
can effectively and efficiently keep the LS healthy and functional with improved communication.
Oh how I love function!
Get Strong! Stay Strong!
Chris